What was the trial about?
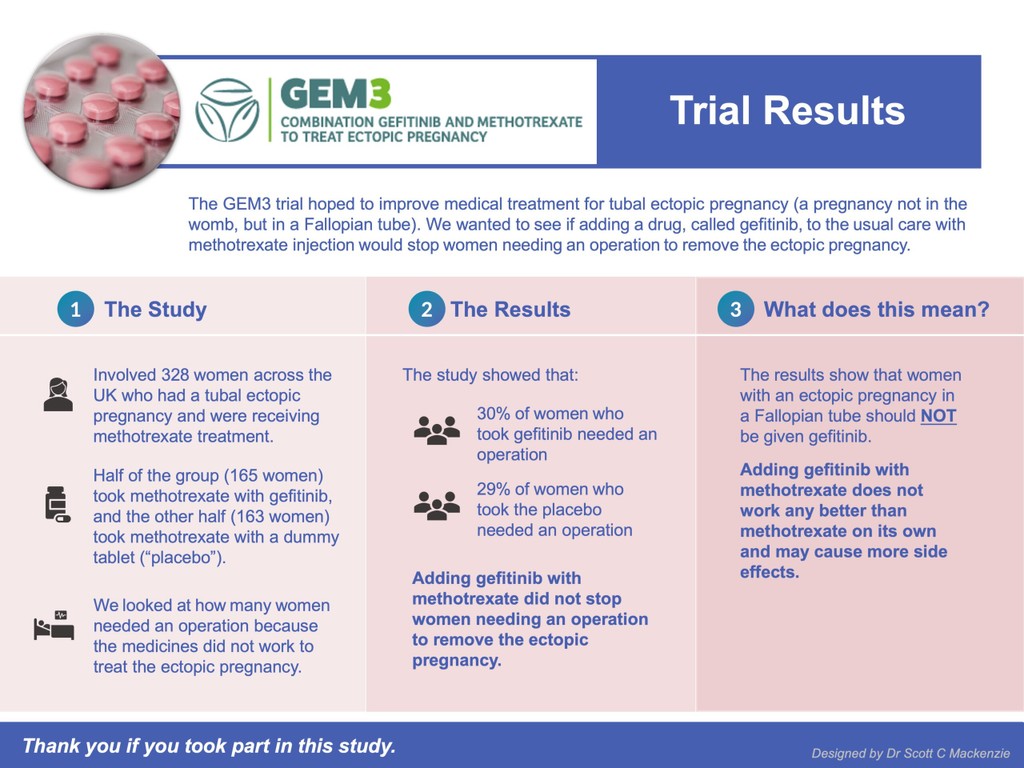
Researchers ran a trial combining gefitinib with methotrexate to treat ectopic pregnancy in a Fallopian tube (GEM3 trial). This was a multi-centre, double-blind, placebo-controlled randomised trial (explanation of these terms below). The results of the GEM3 trial were published in The Lancet on 1 February 2023.
The study involved 328 women across the UK who had a tubal ectopic pregnancy and were receiving methotrexate treatment (medical management). Of the 328 women, 165 took methotrexate with gefitinib while 163 took methotrexate with a dummy tablet (“placebo”). The aim was to assess if a combination of methotrexate and gefitinib reduced the need for surgical treatment of an ectopic pregnancy against using methotrexate on its own.
Explanation of key terms above:
Multi-centre: A clinical trial carried out at more than one hospital or institution.
Double-blind: Women were not told whether they were taking the active medicine (gefitinib) or the placebo and neither were the doctors. This means that both were “blinded” to this information.
Placebo: A dummy drug that had no active ingredients.
Placebo-controlled: Half of the women in the study had the active medicine (gefitinib) and half had the placebo (the “controls”). The medicine looked the same to them and their doctors, but someone else separately recorded which of the women took gefitinib and which took the placebo.
Randomised: Women were given either the treatment drug, gefitinib, or a placebo. The selection was by a secure online computer system so it was “random”.
A randomised control trial is the gold standard of research.
Note: The GEM3 study team recognises that people have diverse gender identities and, in the study report, the word ‘woman’ is used to describe patients or individuals whose sex assigned at birth was female, whether they identify as female, male, or non-binary. The study did not specifically ask questions relating to gender identity.
The results
The trial results showed that 30% of women who took gefitinib needed an operation and 29% of women who took the placebo needed an operation. Adding gefitinib with methotrexate did not stop women needing an operation to remove the ectopic pregnancy.
These results show that women with an ectopic pregnancy in a Fallopian tube (tubal ectopic pregnancy) should NOT be given gefitinib. Adding gefitinib with methotrexate does not work any better than methotrexate on its own and may cause more side effects.
The trial results do provide high-quality information that women with ectopic pregnancies:
- who are treated with methotrexate (with hCG of 1000–5000 IU/L before treatment) take an average of 28 days for the ectopic pregnancy to resolve (when medical treatment is successful);
- require a second dose of methotrexate in 14% of cases;
- require surgery in 29% of cases, despite treatment with methotrexate;
- return to normal menstruation (periods) after an average of 24 days (range of 24–38 days) from the pregnancy ending; and
- who have methotrexate are generally very satisfied with this treatment approach.
This information can be useful for women undergoing methotrexate treatment. There are often many questions around treatment routes particularly if a decision has to be made and this research provides crucial answers to some common queries about methotrexate treatment. It is anticipated that the findings will be rapidly incorporated into international early pregnancy guidelines.
The need to increase awareness and research on ectopic pregnancy
Ectopic pregnancies remain a cause of death of young women. They are worryingly frequent – 1-2% pregnancies are ectopic – and their frequency is rising. Diagnosis and treatment can involve a range of medical professionals including GPs, specialists in emergency medicine, obstetricians and gynaecologists, radiologists and sonographers, pharmacologists, clinical psychologists, midwives, and nurses. However, interest in this common, life-endangering condition in medical and scientific journals appears surprisingly low. Professor Horne hopes that the publication of the GEM3 trial results will raise awareness of ectopic pregnancy and encourage further large-scale research on the condition. He says:
“Ectopic pregnancy is still the commonest cause of death in early pregnancy and, even if not fatal, the effects are distressing and far-reaching. Women can suffer from long term psychological problems and it can impact on their future fertility. If an ectopic pregnancy is diagnosed early, it is likely it can be treated effectively and perhaps avoiding the need for invasive surgery. That’s why it’s important that there is more research like our trial into ways that we can improve the medical management of the condition.”
More information
The trial was run by Professor Andrew Horne at the University of Edinburgh and funded by the National Institute for Health Research (NIHR), supported by the University of Edinburgh, University of Birmingham and NHS Lothian.
Co-investigators are Professor Stephen Tong (University of Melbourne), Professor Siladitya Bhattacharya (University of Aberdeen), Professor Colin Duncan (University of Edinburgh), Professor Arri Coomarasamy (University of Birmingham), Mrs Alexandra Peace-Gadsby (The Ectopic Pregnancy Trust), Professor Jane Daniels (University of Nottingham), Mr Lee Middleton (University of Birmingham), Professor Ben Mol (University of Adelaide), Mr Davor Jurkovic (University College London), Miss Cecillia Bottomley (Chelsea and Westminster Hospital) and Professor Tom Bourne (Imperial College London).
Trial Management Team
Mrs Ann Doust (Research Manager), Dr Magda Koscielniak (Trial Manager), Mr Jordan Doust (Trial Administrator), Mrs Nicola Watson (Specialist Research Nurse), Ms Priscilla Fernandez (Specialist Research Midwife).
You can see a list of the recruiting centres included here:
https://www.ed.ac.uk/centre-reproductive-health/gem3
If you require information or support, please take a look at our treatments page and the ways in which we can help.
How The EPT supports research
Through the support we provide, we hear first-hand accounts from people who experience ectopic pregnancy and their partners who share their lived-experiences. In this way, we are equipped to be able to provide the patients’ voice to inform help inform research. You can read more about the research we have been involved in on our website.