
What is this research about and how will the registry help?
Researchers based at University College London Hospital are seeking to improve care for the diagnosis and treatment for intramural pregnancies.
An intramural pregnancy occurs when an embryo implants within the muscle of the uterus. Intramural pregnancy is also known as intramyometrial pregnancy, myometrial pregnancy, subperitoneal pregnancy, or subserosal pregnancy . An intramural pregnancy is not the same as a correctly-sited pregnancy (where a pregnancy is located in the cavity or “space” of the uterus) or a caesarean section scar ectopic pregnancy.
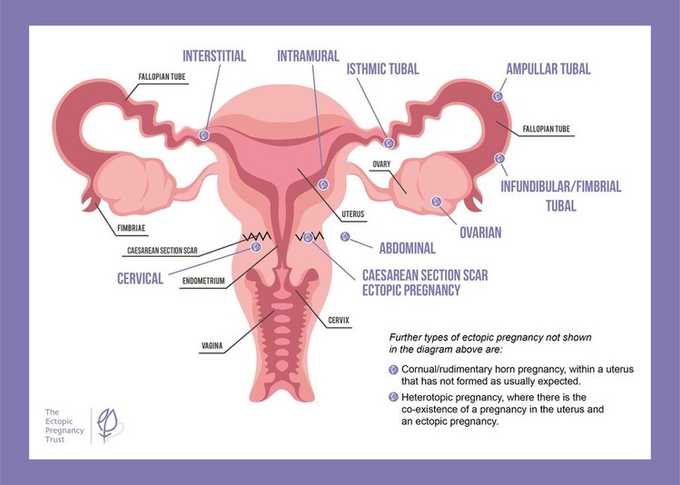
Intramural pregnancy is a rare form of ectopic pregnancy and there is very little research regarding its diagnosis and treatment. The estimated incidence worldwide of ectopic pregnancy is 1–2%, with more than 90% being within a Fallopian tube. Less than 1% of ectopic pregnancies are intramural. Data on intramural pregnancy is very limited, with there being approximately 100case studies. Therefore, there is currently insufficient evidence to create a standard way of diagnosing and treating intramural pregnancy.
To address this data gap, researchers have developed a secure, online data registry for intramural pregnancy cases. By collecting cases of intramural pregnancy from doctors around the world, they aim to study the diagnosis and treatment of the condition. The registry is called the IMP Registry and will be open for at least five years initially. The findings will then be used to identify a standardised method for diagnosis and treatment of intramural pregnancy. The study’s Steering Committee includes a participant who experienced two intramural pregnancies and is patient representative (Ms S) and Munira Oza, Chief Executive of The Ectopic Pregnancy Trust, as patient advocate. Ms S generously shares her experiences and motivations to join this project below.
How you can help this project on intramural pregnancy
If you have experienced an intramural pregnancy, you can help by contacting the research team to let them know. They will then send information to you about the IMP Registry, for you to share with your doctors. This information will invite your doctors to submit your case to the IMP Registry.
You can contact the research team on uclh.impregistry@nhs.net and please provide the following details:
Your name
Your email address
Confirmation that you would like details about the IMP Registry to send to your doctors
Confirmation that you will forward the details about the IMP Registry to your doctors for them to submit your case
Please be aware that the details in the Registry will be anonymous so your doctors will not be including your personal details.
Please note that the IMP Registry is not set up for individuals to input their own cases. The IMP Registry must be completed by your healthcare team, following the information that you forward to them.
The IMP Registry will be open until 31st December 2029 (but this date may be extended) and so deadline for interest in submissions is 1st December 2029.
Ms S’ story
When I was first told I had an ectopic pregnancy, I didn’t expect to hear a term I had never come across before – intramural pregnancy. I was later diagnosed with a further intramural pregnancy so I experienced two of these rare types of ectopic pregnancy just two years apart. In both cases, the initial scans at my local hospital missed the diagnosis, which was only confirmed after I was referred to a specialist centre several hours away.
Because intramural pregnancies are so rare, there was very little reliable information available online to help me understand what was happening. That uncertainty made an already frightening time even harder. My first intramural pregnancy was managed expectantly and took over 12 months to resolve – a long, emotional wait before I could even think about trying again. My second was treated with a local injection of methotrexate under ultrasound guidance, which thankfully worked more quickly but still took several months to completely resolve.
Alongside these two ectopic pregnancies, I have also experienced recurrent miscarriages. I still hope to start a family one day, but these experiences have taken a toll on my mental health. The delays in diagnosis, long journeys for treatment, prolonged recoveries, lack of specialist knowledge locally, and absence of psychological support for me and my partner all made the journey lonelier and more challenging than it needed to be.
That is why I joined the IMP Registry steering committee. I want to help ensure other women don’t have to face the same uncertainty, delays, and isolation I experienced. By collecting and studying more cases of intramural pregnancy, we can help healthcare professionals recognise it sooner, improve treatment, and provide better emotional support for patients and their families. My hope is that, through this work, others will find clearer answers, faster treatment, and greater hope for the future.
Keeping updated
You can follow this research’s progress through dedicated social media channels on X and Instagram:
X: @impregistry
Instagram: impregistry
Support for you
The EPT’s support services are available to anyone affected by ectopic pregnancy, including intramural pregnancy. You are welcome to lean on us if you need and find information on our website: https://ectopic.org.uk/how-we-can-help
