Intrauterine contraceptive devices (IUCDs) and ectopic pregnancy: questions answered
In this article, we explore the causes, symptoms, and treatment options for this rare but important topic and explain how The Ectopic Pregnancy Trust can support anyone going through this traumatic experience. So, whether you are a healthcare provider, someone who uses an IUCD, a partner, a friend, or a relative of someone sadly experiencing an IUCD-related ectopic pregnancy, or you are simply interested in learning more, you can read on and discover what you need to know about IUCD-related ectopic pregnancies.
IUCD related questions
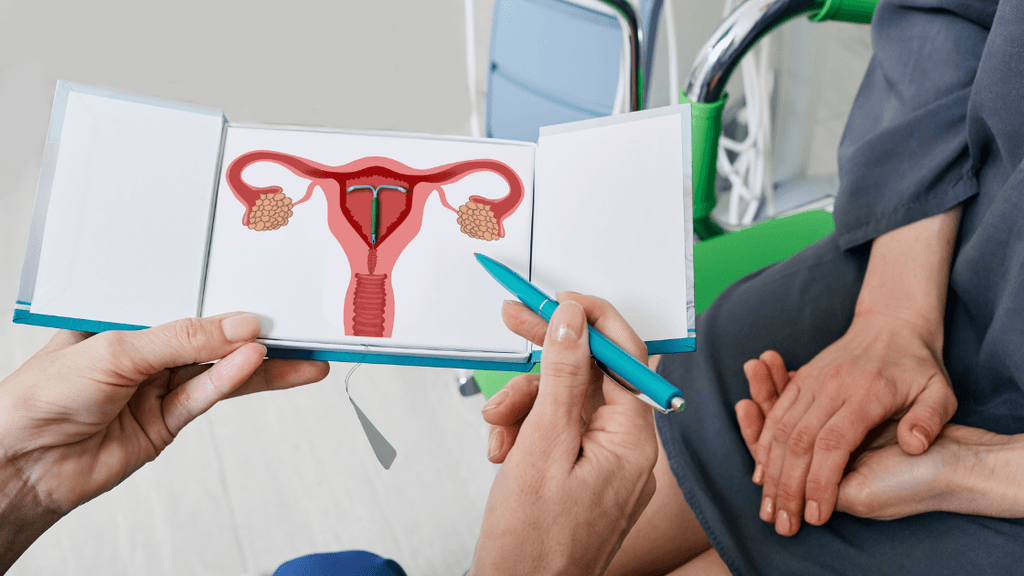
What is an intrauterine device?
An intrauterine contraceptive device (IUCD) is a small, plastic, T-shaped device that is put into the uterus (womb) by a doctor or nurse to stop pregnancy from occurring. It is a form of reversible contraception, like the contraceptive pill, implant, and injection. IUCDs, also known as coils, offer long-lasting birth control and can be left in for 3-10 years, depending on the type, but they can be removed at any time. IUCDs can be hormonal or non-hormonal (copper).
Hormonal IUCDs (also known as intrauterine systems or IUS, such as Mirena, Jayness) prevent pregnancy by releasing a synthetic progesterone called levonorgestrel hormones, making it inhospitable to sperm and pregnancies. Non-hormonal IUCDs contain copper and work similarly by releasing copper ions. IUCDs are more than 99% effective at preventing pregnancy.
Can an IUCD cause an ectopic pregnancy?
Unfortunately, IUCDs can fail in around 1% of cases and do come with a risk of pregnancy.
If an IUCD is kept in place past its recommended removal deadline, it is not guaranteed to prevent pregnancy, and other forms of contraception should be used until it can be removed. IUCD pregnancies can also happen due to IUCD ‘expulsion’, where the IUCD falls out, or if it moves out of place from the top of the uterus where it should sit. Finally, there is a high risk of pregnancy with a hormonal IUCD that has not started to work yet; backup contraception should be used for the first seven days after getting the hormonal IUCD put in. Copper IUCDs work immediately after insertion.
If you do get pregnant with an IUCD, it is more likely to be an ectopic pregnancy. This is because IUCDs are so effective at preventing pregnancies in the uterus, if a pregnancy does occur, it is more likely to occur outside of the uterus. IUCD-related ectopic pregnancies can be very traumatic and confusing. Lily experienced an ectopic pregnancy while using an IUD, and shared her experience with The Ectopic Pregnancy Trust:
“I had very confused feelings since the pregnancy was not planned, yet I still felt an immense sense of loss and grief”.
We understand the complicated feelings that come with IUCD-related ectopic pregnancy and we are here to support anyone going through this. If you need support yourself, or know someone that you think needs our help, please do read more about how The EPT can help.
How could an IUCD cause an ectopic pregnancy?
The IUCD does not directly cause ectopic pregnancy; rather, it prevents typical intrauterine pregnancies (normally-sited), but it does not prevent ectopic pregnancies. Copper IUCDs are thought to also increase the risk of ectopic pregnancy by causing inflammation in the Fallopian tubes. Both types of IUCD, particularly during insertion and for the first 20 days, may lead to irritation or infection of the Fallopian tubes. Keeping an IUCD past its removal date also increases the risk of infection.
An ectopic pregnancy occurs when a fertilised egg implants and grows outside the uterus (womb). Most commonly, an ectopic pregnancy occurs in one of the Fallopian tubes, which carry eggs from the ovaries to the uterus; also known as a tubal pregnancy. Ectopic pregnancies can also occur in the cervix, abdomen, or ovary. Tubal pregnancies occur when the fertilised egg gets stuck in a Fallopian tube on its way to the uterus. The egg may get stuck due to the Fallopian tube being misshapen, inflamed, or otherwise damaged (for example, due to scarring), and hormonal imbalances may also play a part. Risk factors include previous ectopic pregnancy, pelvic inflammatory disease (PID), certain sexually transmitted infections (STIs), previous pelvic, abdominal, or Fallopian tube surgery, and endometriosis.
How likely is it to have an ectopic pregnancy with an IUCD?
A review of IUCD safety and efficacy stated that ectopic pregnancies affect 2 in 10,000 women with hormonal IUCDs, and 5 in 10,000 copper IUCD users, each year. That corresponds to 0.02% and 0.05%, respectively. Comparatively, the overall incidence of ectopic pregnancy in the UK is 1.25% (1 in 80). So although the pregnancy itself is more likely to be ectopic when the woman has an IUCD, the chance of getting pregnant is much lower, meaning the overall risk of ectopic pregnancy is drastically reduced.
Is ectopic pregnancy common after IUCD removal?
Though an IUCD does increase the chance of a pregnancy being ectopic while it is in place, there is no increased risk of ectopic pregnancy after IUCD removal. In fact, there is no higher risk of any pregnancy complications after IUCD removal. In most cases, IUCD removal or previous IUCD use does not affect fertility. However, in the very rare cases that there is scarring in the uterus from the IUCD, particularly following an infection, this may reduce the chances of becoming pregnant and having a viable pregnancy.
IUCDs are safe and mostly very easy to remove. Removal will be carried out by a medical professional. Although IUCDs are effective and can stay in place for between 3 and 10 years, they can be removed at any time. Generally, it will be removed by pulling the threads with forceps. However, if the IUCD threads snap or cannot be reached, it will need to be removed by ultrasound-guided removal or a removal procedure known as a hysteroscopy.
What are the signs of ectopic pregnancy with an IUCD?
Signs of early ectopic pregnancy may be very similar or identical to the usual signs of pregnancy:
- A missed period
- Nausea
- Vomiting
- Tender or swollen breasts
- Increased urination
- Fatigue
Additional symptoms associated with ectopic pregnancies may also be experienced. These include:
- Pelvic pain or abdominal pain or discomfort
- Vaginal bleeding or an abnormal period
Ectopic pregnancies can lead to rupturing of the Fallopian tube, which can have life-threatening consequences. Symptoms of this should be treated as a medical emergency, and include:
- Heavy bleeding
- Pain at the tip of the shoulder
- Pain or pressure in the rectum
- Sharp, sudden pains or cramping in the stomach
- Extreme lightheadedness or dizziness
- Fainting
- Shock
- Looking extremely pale
What to do if you have signs of ectopic pregnancy with an IUCD?
If you are at all worried about any symptoms you are experiencing, you should contact a healthcare practitioner as soon as possible. They will be able to refer you to your local Early Pregnancy Unit (EPU) for assessment and do a pregnancy test (if not already done so). The EPU would diagnose whether or not a pregnancy is ectopic and recommend the best course of action. If you are experiencing symptoms of Fallopian tube rupture, you should seek emergency medical help immediately.
How is an ectopic pregnancy with an IUCD treated?
The recommended treatments for ectopic pregnancy with an IUCD in the UK are surgical or medical treatments. Sometimes, in cases where the pregnancy hormone (beta hCG) levels are dropping quickly, expectant management may be considered. Generally, the IUCD will first be removed, however, there have been cases where ectopic pregnancy was treated and the IUCD kept in place.
Case studies have shown that the most effective way of managing an ectopic pregnancy with an IUCD is surgery. Keyhole surgery (laparoscopy) will be carried out to remove the pregnancy and sometimes the affected Fallopian tube. You may also be given an anti-D injection after surgical treatment.
In certain situations, medical management may be appropriate. A drug called methotrexate is used, which stops the pregnancy from developing any further. This is most appropriate in early ectopic pregnancies, where there are low levels of pregnancy hormones and there are no signs of rupture like worrying pain or bleeding.
Where pregnancy hormone levels are low and there are no signs of rupture, surgery or medical interventions may not be required. Instead, expectant management may be offered, which entails closely monitoring pregnancy hormone levels to ensure they continue to drop to non-pregnant levels, indicating that the pregnancy has ended naturally.
You can read more about the different types of treatment here. It is important to give yourself time to recover both physically and emotionally following an ectopic pregnancy, and The Ectopic Pregnancy Trust will do all we can to support you in the healing process.
How can The Ectopic Pregnancy Trust support you through an ectopic pregnancy with an IUCD?
If you experience an IUCD-related ectopic pregnancy, The Ectopic Pregnancy Trust is here to support you. The Ectopic Pregnancy Trust aims to provide information and support to everyone affected by ectopic pregnancy and other early pregnancy complications, and the healthcare professionals who care for them. The Ectopic Pregnancy Trust also hopes to advance education and promote awareness of ectopic pregnancy and other early pregnancy complications among the medical profession and the wider public. Finally, The Ectopic Pregnancy Trust hopes to support research into ectopic pregnancy and other early pregnancy conditions.
Other pages you may find helpful
Find out about different treatment options including expectant management, medical management with methotrexate, and surgical treatment
Read more here about ectopic pregnancy symptoms
Read more about the reasons and risk factors for an ectopic pregnancy
If you have experienced ectopic pregnancy, we are here to support you