Think Ectopic - Resources for sites
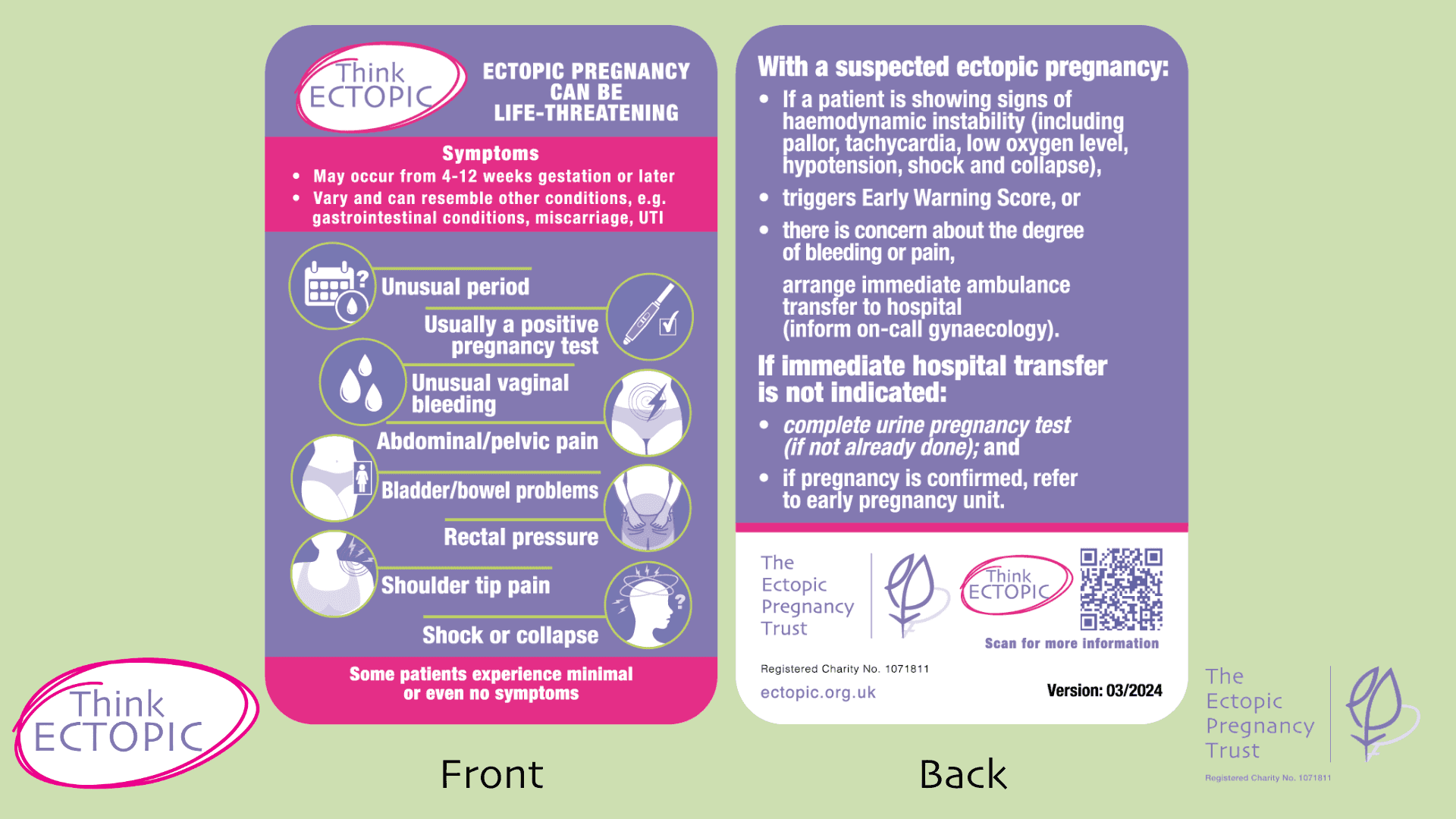
This ectopic pregnancy biocard is an easy-to-use patient safety tool. It highlights signs of ectopic pregnancy and next steps for symptomatic women/people. To order copies of biocards for urgent and primary care colleagues, please complete the form below.
Take a look at the new Think Ectopic biocard and order copies for your hospital/clinic below
Think Ectopic biocard
The ectopic pregnancy biocard is an easy-to-use patient safety tool. It highlights signs of ectopic pregnancy and next steps for symptomatic women/people.
Keep the biocard to hand as a helpful reminder to bear in mind and consider the condition. It can be slotted into your lanyard holder or clip it in through the slot. Made of durable plastic, it is hard-wearing and can be wiped clean.
If you are a healthcare professional and would like to know how to obtain hard copies, please get in touch through the form below. We will respond with details of the relevant contact person at your setting.
To order copies of biocards, please complete the form at the bottom of this page.
Think Ectopic videos
This three-part video series contains further information about ectopic pregnancy. Topics are:
- What is an ectopic pregnancy?
- How to spot an ectopic pregnancy.
- What to do if you suspect an ectopic pregnancy.
The videos powerfully include lived experiences from women and people who have experienced ectopic pregnancy.
Conducting a urine pregnancy test - key points to avoid false negatives
Healthcare professionals will be very familiar with conducting pregnancy tests with patients. To obtain accurate results, here are a few handy reminders.
- Use a concentrated urine sample
It is preferable to test with the first urine of the day and in urine which has been in the bladder for at least four hours. The first urine of the day is when urine is most concentrated. However, when completing a urine pregnancy test to determine pregnancy where a symptomatic woman or person presents, do not wait for the next morning to conduct the test. It is important to conduct a pregnancy test as soon as possible to enable quick referral. Ask the patient not to drink too much fluid before the pregnancy test as this can dilute the hCG in the urine.
- Avoid using a contaminated urine sample
Let your patient know to take the urine sample with care and to try to avoid any blood being mixed in with it. Do check the sample provided by your patient and, if it is a contaminated sample, the test should be re-done.
- Follow instructions on pack carefully
Check the expiration date on the pregnancy test and read the manufacturer’s directions for conducting the pregnancy test. There are numerous pregnancy test brands and they may differ in how the urine sample needs to be added to the test, timeframe for looking at the result window, and interpreting the result. Do familiarise yourself with the pregnancy test used in your department. If the brand has changed or if you are unsure, ask for advice from a colleague.
- Useful reminders for conducting the pregnancy test
While healthcare professionals will of course be familiar with how to conduct a pregnancy test, here are a few helpful points to help with getting an accurate result.
- Supplies needed for a urine pregnancy test:
• Disposable sample pot for patient to catch urine
• Pregnancy test
• Timer, such as on phone or watch
• Gloves while you handle the urine sample and conduct the test
• Appropriate bins to dispose of contaminated waste per local infection control policies
- Conducting urine pregnancy test:
1. Obtain consent from your patient to conduct the test and explain why it is needed.
2. Check the expiration date on the test and ensure you are familiar with how to conduct the test according to manufacturer’s instructions.
3. Wash your hands and put on gloves before handling the urine sample pot.
4. Use the dropper to remove some urine from the patient’s sample pot.
5. Drop the required amount of urine onto the test area. The location of the test area can vary depending on brand so take a look at the instructions. Usually the amount of urine needed is three drops, but do check manufacturer’s instructions.
6. Keep the test on a flat surface.
7. Wait for results by setting a timer. The time will be according to manufacturer’s instructions. Do not read the test after the allotted time has passed.
8. Interpret results according to pregnancy test instructions.
9. Dispose of equipment in accordance with local infection control policies.
10. Remove and dispose of gloves and wash hands.
11. Report the result to patient and document the result in medical notes. We have more information on our website on safe handover of patient information using the SBAR tool and safety netting advice. See below for pro forma,
12. A positive pregnancy test does not necessarily indicate a viable pregnancy and cannot identify where the pregnancy is located.
- Interpreting the result:
Most pregnancy tests have two display areas labelled with C and T.
C stands for control. A line should appear against this to show that sufficient urine was added to the test and the test is working.
T stands for test. This is where the test result will display with a line if test is positive.
Positive: A positive pregnancy test is shown with two lines. There will be one line in the Test area and one line in the Control area. The test has detected hCG in the urine sample. It does not matter how strong or faint the line is in the Test area and any line is a positive result.
Negative: A negative pregnancy test is shown with one line. There will be a single line in the Control area and no line in the Test area. This means that the test has not detected hCG in the urine sample.
Invalid: An invalid pregnancy test is shown with one line in the Test area and no line in the Control area. This means that the test has not been conducted properly and it should be repeated following the steps above.
If patient has a positive result: and has symptoms of ectopic pregnancy, refer immediately to your early pregnancy unit.
If the patient is haemodynamically unstable (tachycardia, hypotension, low oxygen levels, shock and collapse or recent collapse), call 999 for emergency transfer to the nearest A&E, advising call handlers that this is a possible ruptured ectopic pregnancy, and providing most recent clinical observations.
We have information on handover of patient information using SBAR communication tool (Situation, Background, Assessment, Recommendation). See below for pro forma.
If patient has a negative result: and has symptoms of ectopic pregnancy, repeat the pregnancy test and refer to your early pregnancy unit for review.
SBAR handover – Situation, Background, Assessment, Recommendation
The Healthcare Safety Investigation Branch’s report on the diagnosis of ectopic pregnancy included a safety recommendation on improvement for information that should be provided to early pregnancy units to identify those most as risk from ectopic pregnancy and consequent deterioration. This SBAR pro forma can assist with providing information on handover between departments or to senior colleagues for patients whose health is deteriorating or where there is concern.
This pro forma needs to be completed by filling out the relevant details for your patient. There are spaces within the pro forma that you must complete before handing to your colleagues.
Please note: This pro forma is for general information only. It does not replace individual information, diagnosis, or advice given by an appropriately qualified healthcare professional. You must apply your clinical judgement in the provision of information generally to your colleague, whether using this pro forma or otherwise. Although we make reasonable efforts to update the information on this pro forma, we make no representations, warranties, or guarantees, whether express or implied, that the content is accurate, complete, or up to date.
Safety netting discharge advice
The Healthcare Safety Investigation Branch report on diagnosis of ectopic pregnancy included safety recommendation on the provision of information following discharge from the emergency department with an early pregnancy problem while awaiting further assessment by early pregnancy services.
This pro forma can assist with providing patients with written information following discharge from primary or urgent/acute care while awaiting further assessment by early pregnancy services.
This pro forma needs to be completed by filling out the relevant details for your unit/setting. There are spaces within the pro forma that you must complete before distributing to your patients. If you require an editable version, please get in touch.
You can provide this to your patients electronically or print and hand out.
Please note: This pro forma is for general information only. It does not replace individual information, diagnosis, or advice given by an appropriately qualified healthcare professional. You must apply your clinical judgement in the provision of information generally to your patient, whether using this pro forma or otherwise. Although we make reasonable efforts to update the information on this pro forma, we make no representations, warranties, or guarantees, whether express or implied, that the content is accurate, complete, or up to date.
Symptoms of ectopic pregnancy in A4 poster format (landscape)
Symptoms of ectopic pregnancy with accompanying images that can be displayed on screens or printed and added to clinic noticeboards.
Symptoms of ectopic pregnancy in A4 poster format (portrait)
Symptoms of ectopic pregnancy with accompanying images that can be displayed on screens or printed and added to clinic noticeboards.
Think Ectopic Champion resources
Download your FREE social media images, posters, badges and suggested social media copy to show your support for the Think Ectopic campaign. By spreading the word we can save lives together!
Resources include:
-Think Ectopic Champion badges for use on social media/webpages
-Think Ectopic printable posters
-Think Ectopic Champion social media graphics
-Suggested social media copy
We had a lady recently who sat in cohort and they [the paramedics] thought she was a UTI or pulmonary embolism - as soon as they did a pregnancy test within minutes she was in the right place and within an hour, she was in theatre. It's almost as if and up until that pregnancy test, they were thinking all sorts and then the moment they knew she was pregnant, they went straight to an ectopic. The ambulance crew said that was on the back of the biocard.- Feedback from pilot site lead
Find out more about the Think Ectopic campaign
Receive FREE Think Ectopic biocards for healthcare professionals and be a Think Ectopic champion! Please get in touch by completing the form below. We will get in touch with next steps.
The biocards are aimed at urgent and primary care staff. Thank you for your help in distributing them among your colleagues.
Note: For UK-based healthcare professionals only.
Professional guidance and reports
NICE Guidance, Ectopic pregnancy and miscarriage: diagnosis and initial management, NG126
RCOG Green-top Guidelines: Diagnosis and Management of Ectopic Pregnancy: Green-top Guideline 21
MBRRACE Maternal Report 2022, “Saving Lives, Improving Mothers’ Care”
MBRRACE-UK Maternal Report 2019, “Saving Lives, Improving Mothers’ Care”
MBRRACE-UK Maternal Reports 2024, “Saving Lives, Improving Mothers’ Care”